Hip Care
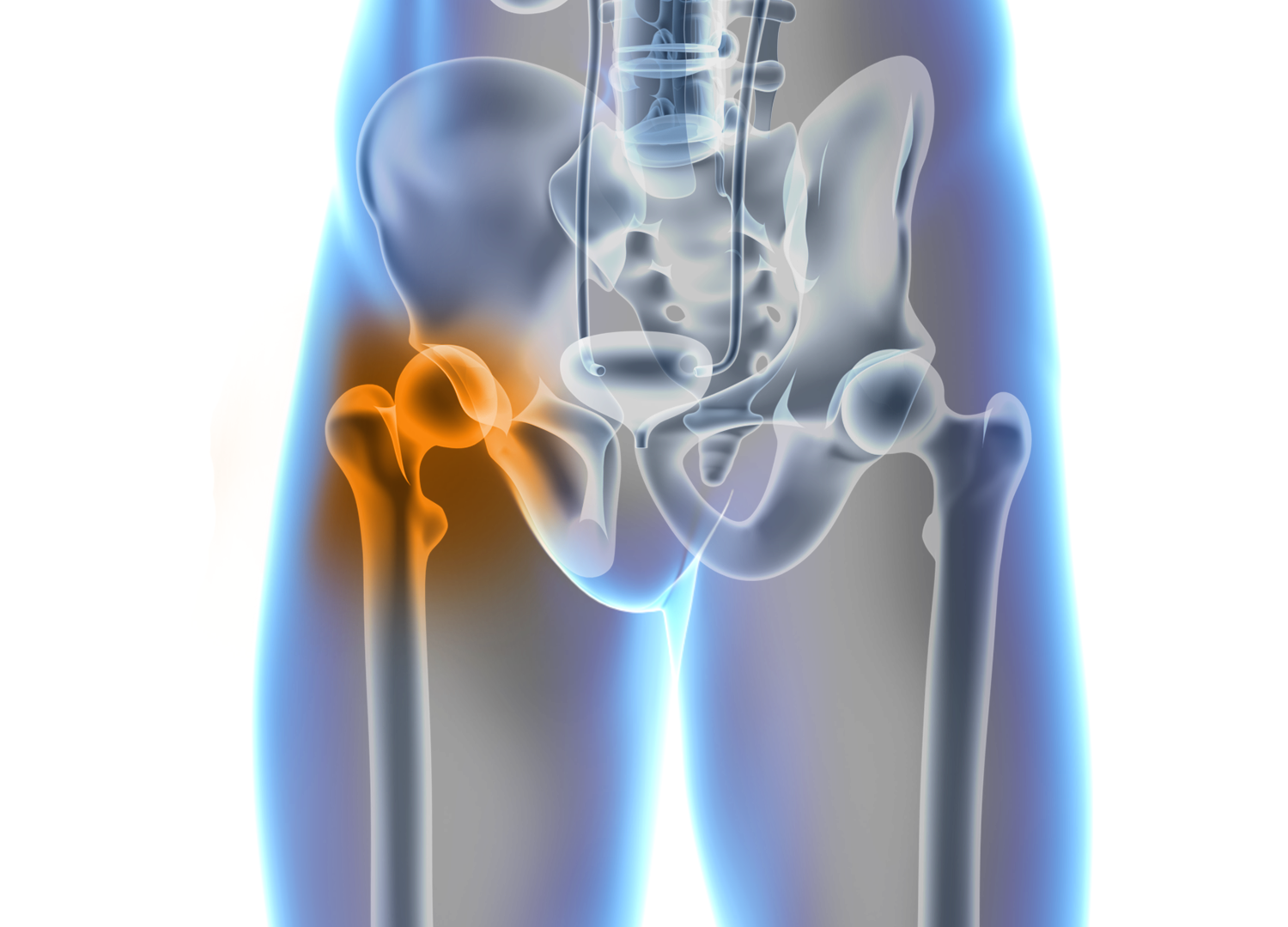
Your hip joint is an incredible masterpiece of biomechanics, granting you the power to move, explore, and thrive in your daily life. Should you face the challenges of hip discomfort and restricted mobility, envision the transformative potential of hip replacement surgery. Embrace the journey towards a future free from hip pain and take that initial stride towards a more active and pain-free life.
Hip Care Information












